7800 SW 87 AVE SUITE B-270 MIAMI, FLORIDA 33173
Contact Us
- Home
- Corneal Dystrophy and Degeneration
Corneal Dystrophy and Degeneration
Corneal dystrophy and degeneration are groups of eye conditions characterized by the abnormal accumulation of substances in the cornea, causing structural changes and functional impairments. They can affect one or several layers of the cornea, lead to visual disturbances, and in some cases, significant vision loss.
Steven Johnsons Syndrome (SJS) is a severe skin reaction, often to medication, that can also have ocular manifestations. SJS can cause serious damage to the ocular surface, including the cornea, and is associated with long-term ocular complications, such as dry eyes, corneal ulcers, and visual impairment.
Autoimmune diseases, where the body’s immune system mistakenly attacks its own cells, can also affect the eyes, particularly the cornea. Conditions such as rheumatoid arthritis, Sjögren’s syndrome, and systemic lupus erythematosus can lead to corneal inflammation, dryness, ulcers, and scarring.
Given the complexity and diversity of these conditions, their management requires expertise and an individualized approach, something Dr. Edward Boshnick, an esteemed optometrist specializing in complex eye disorders, excels in.
Steven Johnsons Syndrome (SJS):
Steven Johnsons Syndrome is an uncommon, severe reaction to medication or infection. This condition is considered a medical emergency, and it primarily involves the skin, mucous membranes, and eyes. In SJS, the immune system responds aggressively to a trigger, leading to severe skin blistering and peeling.
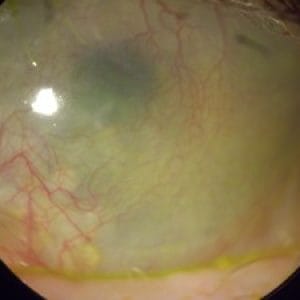
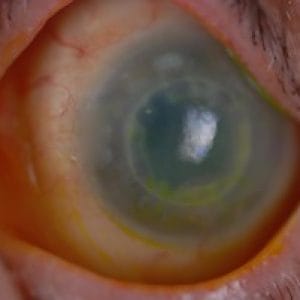
When it comes to ocular manifestations, SJS can have serious and debilitating consequences. The aggressive immune response can attack the surface of the eyes, including the cornea, causing severe ocular surface disease. Acutely, SJS can cause conjunctivitis, eyelid skin shedding, and corneal blisters or erosions. If not managed quickly, this can lead to corneal ulcers, perforations, and eventually, loss of vision.
Long-term ocular complications of SJS include chronic dry eye, symblepharon (adhesion of the eyelid to the globe), trichiasis (inward-growing eyelashes), corneal neovascularization, corneal scarring, and severe visual impairment. The damage caused by SJS is often irreversible, making prevention and early detection crucial.
Rheumatoid Arthritis (RA):
Rheumatoid Arthritis is a systemic inflammatory disease that primarily affects the joints, causing pain, swelling, stiffness, and progressive damage. However, RA can also have significant ocular manifestations, with the cornea being one of the areas it can impact. Keratitis sicca, or dry eye, is the most common eye complication of RA. This is caused by the decreased production of tears or increased tear evaporation, leading to damage to the corneal surface, reduced vision, and significant discomfort. More severely, RA can cause peripheral ulcerative keratitis, a serious condition that involves inflammation and ulceration of the cornea, potentially leading to vision-threatening complications.
Sjögren's Syndrome:
Scleral lenses are large gas permeable lenses that vault over the cornea without touching it. They rest on the sclera, which is the white portion of the eye, making them incredibly comfortable for the wearer. A special fluid fills the space between the back portion of the lens and the front of the cornea, creating a liquid environment that promotes corneal healing. As such, scleral lenses are deemed medically necessary for treating the aforementioned conditions.
Systemic Lupus Erythematosus (SLE):
Systemic Lupus Erythematosus is a systemic autoimmune disease that can affect virtually any organ in the body, including the eyes. While less common than in RA and Sjögren’s syndrome, SLE can also cause ocular complications. The inflammation from SLE can lead to keratitis, or inflammation of the cornea, which can result in pain, redness, light sensitivity, and blurred vision. In severe cases, persistent inflammation can lead to the development of corneal ulcers and scarring, which can significantly affect vision.
These conditions often require a multidisciplinary approach to care. Treatment typically involves systemic medications to manage the underlying autoimmune disease, local therapies to manage ocular symptoms (such as artificial tears, anti-inflammatory eye drops, or punctal plugs to reduce tear drainage), and specialized contact lenses, such as scleral lenses, to protect the cornea and promote healing.
Types of Corneal Dystrophies
Corneal dystrophies are a group of genetic eye disorders characterized by the abnormal accumulation of substances in the cornea, which can result in vision loss. Although there are many types of corneal dystrophies, they are generally categorized by which layer of the cornea they affect – the epithelium and Bowman’s layer, the stroma, or Descemet’s membrane and the endothelium. Below, we delve into some of the more common types:
1. Epithelial-Basement Membrane Dystrophy (EBMD): Also known as map-dot-fingerprint dystrophy, EBMD affects the epithelium, the outermost layer of the cornea. In EBMD, the epithelial basement membrane develops abnormally, leading to the formation of tiny maps, dots, and fingerprint-like lines on the cornea. This condition often causes recurrent corneal erosion, where the epithelial cells periodically break loose, causing severe pain, sensitivity to light, and blurry vision.
2. Fuchs’ Endothelial Corneal Dystrophy (FECD): This affects the endothelium, the innermost layer of the cornea, and Descemet’s membrane. In FECD, endothelial cells gradually die off, causing fluid build-up within the cornea leading to corneal swelling, and ultimately, vision loss. This is the most common form of corneal dystrophy and it often becomes noticeable in people in their 30s and 40s, although significant vision problems often do not appear until people reach their 50s or 60s.
3. Lattice Corneal Dystrophy: This primarily affects the stroma, the middle and thickest layer of the cornea. In lattice dystrophy, abnormal protein fibers accumulate in the stroma, creating a lattice-like pattern that can cloud the cornea and interfere with vision. There are several types of lattice dystrophy, each associated with different symptoms and levels of severity.
4. Granular Corneal Dystrophy: This also affects the stroma. In granular dystrophy, granular deposits accumulate in the corneal stroma, which appear as small, round white dots scattered across the cornea. Over time, these dots can grow and merge, leading to vision impairment.
5. Macular Corneal Dystrophy: This is a relatively rare form of corneal dystrophy that also affects the stroma. In macular dystrophy, abnormal deposits accumulate throughout the stroma, as well as in Descemet’s membrane and the endothelium. This can cause severe vision loss.
It is important to note that symptoms, prognosis, and treatment options vary depending on the type of corneal dystrophy. Additionally, while some people with corneal dystrophies experience significant vision problems, others may remain asymptomatic. Treatments for corneal dystrophies can range from using lubricating eye drops to manage symptoms to corneal transplantation in severe cases.
Dr. Edward Boshnick's Approach to Treatment
Dr. Boshnick utilizes a non-invasive approach to treating eye conditions, including corneal dystrophy, degeneration, and issues arising from SJS and autoimmune diseases. He emphasizes the importance of a thorough diagnosis, patient education, and customized treatment plans.
In cases of corneal dystrophy and degeneration, Dr. Boshnick may employ specially designed contact lenses, including scleral lenses, which can improve vision by creating a smooth optical surface over the irregular cornea. These lenses also provide a nurturing environment for the cornea, facilitating healing and offering protection.
For patients with SJS and related ocular surface diseases, Dr. Boshnick often uses prosthetic scleral devices, also known as PROSE (Prosthetic Replacement of the Ocular Surface Ecosystem) treatment. These custom-made prosthetic lenses vault over the compromised cornea and protect the damaged ocular surface, providing both visual rehabilitation and comfort.
When treating ocular manifestations of autoimmune diseases, Dr. Boshnick’s approach aims to manage the underlying condition, alleviate symptoms, and prevent further damage to the eyes. He works closely with other healthcare providers to ensure patients receive the most comprehensive care.
Scleral Lenses:
Scleral lenses are large-diameter gas permeable contact lenses that rest on the sclera, the white part of the eye, and vault over the entire corneal surface. This design creates a fluid-filled space between the back surface of the lens and the cornea, which can dramatically improve comfort and visual acuity in patients with irregular corneal surfaces.
Protection of the Cornea:
Scleral lenses can serve as a protective shield for the cornea, preventing mechanical damage from the environment or the blinking action of the eyelids. This is particularly beneficial in cases where the cornea is fragile due to inflammation, dryness, or scarring.
Promoting Healing:
The fluid reservoir behind the scleral lens helps to keep the cornea constantly bathed in a soothing saline solution. This moist environment can promote healing of the corneal surface, helping to alleviate symptoms like dryness, burning, and discomfort, and may help to heal corneal ulcers or erosions that are common in conditions like rheumatoid arthritis, Sjögren’s syndrome, and systemic lupus erythematosus.
Improving Visual Acuity:
As the scleral lenses vault over the irregular cornea, they essentially replace the irregular corneal surface with a perfectly smooth optical surface, thereby improving the focus of light into the eye. This can significantly enhance visual acuity in patients who have visual distortion due to corneal irregularities.
Dr. Boshnick’s extensive experience in fitting scleral lenses allows him to customize the lens design to each patient’s unique eye shape and condition. His personalized approach ensures that the lenses provide the maximum benefit in terms of comfort, corneal health, and visual improvement. Regular follow-ups ensure that the lenses continue to fit well and provide the intended benefits over time.
The use of scleral lenses for these challenging corneal conditions represents a significant advancement in non-surgical eye care and allows patients to experience improved visual acuity and comfort. Dr. Boshnick’s expertise with these lenses makes him a valuable resource for patients with these complex eye conditions.
Your Vision, Our Priority:
Schedule Your Consultation Now
Frequently Asked Questions
Scleral lenses provide a smooth optical surface, bypassing the irregularities of the corneal surface due to various conditions. This improves vision clarity and provides relief from discomfort. The fluid-filled space between the lens and cornea also keeps the cornea moist, helping to alleviate symptoms of dryness and irritation.
Yes, these conditions can lead to inflammation, dryness, ulcers, and scarring of the cornea. Scleral lenses can protect the cornea, promote healing, and improve visual acuity, providing significant relief for patients with these systemic diseases.
Scleral lenses replace the irregular corneal surface with a perfectly smooth optical surface, which improves the focus of light into the eye. This can significantly enhance visual acuity in patients who have visual distortion due to corneal irregularities.
Yes, most patients find scleral lenses comfortable as they rest on the less sensitive sclera, not the cornea. The cushion of fluid between the lens and the eye also enhances comfort.
Dr. Boshnick takes detailed measurements of each patient’s eyes to design scleral lenses that match their unique eye shape and condition. This personalized approach helps ensure the lenses provide maximum comfort and visual improvement.
Like all contact lenses, scleral lenses need to be cleaned and disinfected daily to keep them safe and comfortable to wear. Dr. Boshnick provides detailed instructions on how to care for scleral lenses.
While scleral lenses cannot stop the progression of these conditions, they can help manage symptoms, protect the cornea, and improve vision quality. Regular monitoring by Dr. Boshnick can ensure the continued effectiveness of the treatment.
Schedule Your Consultation with
Dr. Boshnick
-
-
-
7800 Sw 87 Ave Suite B-270
Miami, Florida 33173